Impact of E-Cigarette Smoke on Cardiovascular Function
Cigarette smoking is one of the primary risk factors for cardiovascular disease (CVD). In fact, the American Heart Association reports that smoking-related diseases are responsible for > 440,000 deaths in the US each year. Cigarette smoke contains hundreds of chemical toxicants, which can damage the cardiovascular system, and increase the risk of developing atherosclerosis. Atherosclerosis is caused by plaque buildup in the arteries that can harden and narrow the diameter of the vessel over time and restrict the flow of oxygenated blood throughout the body.
To mitigate some of the harmful effects of tobacco cigarettes, next-generation tobacco and nicotine products (NGPs) such as electronic cigarettes (e-cigarettes) and tobacco heating products (THPs) are available commercially, which have decreased levels of chemical toxicants. However, exposure to e-cigarette smoke still negatively impacted cardiovascular health, albeit to a lesser degree than tobacco smoke. Monocyte activation and adhesion to the vascular endothelium are implicated as one of the key steps in the development of atherosclerosis but how NGPs affect vascular endothelial cell function, inflammation and monocyte activation are not well understood and require further investigation.
The authors of the featured publication established a more physiologically relevant high-throughput in vitro microfluidic cardiovascular model to study the impact of e-cigarette exposure on the development of atherosclerosis.
The Lifeline® catalog has a variety of high-quality endothelial and cardiac cells to enable your cardiovascular research and more including:
- Cardiac microvascular endothelial cells
- Cardiac fibroblasts
- Pulmonary artery endothelial cells
- Aortic endothelial cells
- Coronary artery endothelial cells
- Lung microvascular endothelial cells
- Dermal microvascular endothelial cells (adult and neonatal)
- Iliac artery endothelial cells
- Umbilical cord endothelial cells (HUVECs; primary and 10-donor pool)
New Research Using Lifeline Endothelial Cells
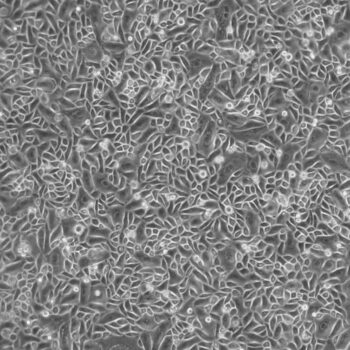
Makwana and Colleagues designed a new in vitro model that utilizes microfluidics to mimic vascular flow to understand the effects of e-cigarette smoke on monocyte adhesion and vascular endothelial cell function compared to tobacco cigarettes in more physiologically relevant conditions. The high-content BioFlux system utilizes 24- or 48-well microplates fitted with microfluidic channels with tunable flow rates and high-resolution fluorescent microscopy. Lifeline’s Primary Human Aortic Endothelial cells (HAECs), grown in VascuLife® VEGF Endothelial Cell Culture Medium with VEGF LifeFactors, were used to establish monolayers in the microfluidic channels. Monocyte adhesion was quantified by flowing a suspension of monocytic THP-1 cells through the channels. To validate the assay, HAECs were pre-treated with TNFα, a known pro-inflammatory cytokine. THP-1 monocyte adhesion to HAECs was successfully observed and quantifiable in the BioFlux microfluidic system in response to TNFα treatment. TNFα was used as a positive control for monocyte adhesion in subsequent assays along with the vehicle-only negative control.
Whole smoke conditioned media (WSCM) and electronic cigarette vapor (from a Vype ePen) conditioned media (eVCM) were generated for the monocyte adhesion assay. Endothelial cells were exposed to either WSCM, eVCM, or nicotine across a range of non-toxic concentrations (15, 150, and 1500 ng/mL nicotine equivalents (n.e.)) for 24 h alongside +/- controls prior to assessing monocyte adhesion after a 40-min incubation period. THP-1 cell adhesion to HAECs was found to be elevated for both WSCM and eVCM with a 3-fold and a 1.6-fold increase at the highest exposure concentration (1500 ng/mL n.e.), respectively. HAEC exposure to nicotine-induced no notable increase in THP-1 adhesion.
After confirming the upregulation of monocyte adhesion resulting from cigarette smoke, the molecular mechanism was investigated using immunofluorescence microscopy and Western blotting to look at protein expression of endothelial adhesion molecules ICAM-1, VCAM-1, and E-Selectin in HAECs after WSCM, eVCM, or nicotine exposure. Only ICAM-1 levels were upregulated in HAECs exposed to WSCM and no significant upregulation of any of the adhesion molecules was detected in the eVCM or nicotine conditions. Confocal microscopy confirmed the ICAM-1-mediated THP-1 cell-to-HAEC adhesion response in WSCM-treated conditions where co-localization of endothelial cell ICAM-1 and monocyte-expressed CD11b on the cell surface was observed. ICAM-1 siRNA knockdown to deplete ICAM-1 levels in the WSCM-treated HAECs reduced monocyte adhesion to levels comparable to the negative control provided further support that WSCM-induced THP-1 cell adhesion to HAECs is predominately mediated through ICAM-1/CD11b.
The results of the study reveal that tobacco cigarette smoke increases monocyte adhesion to the vascular endothelium preferentially through the ICAM-1-CD11b pathway. The results also suggest that an alternate molecular mechanism drives monocyte adhesion in eVCM conditions since ICAM-1 depletion did not result in any such reductions in THP-1 cell adhesion to HAECs as was observed with WSCM. This study successfully validated the BioFlux microfluidics system that, in combination with the THP-1 cell adhesion assay, represents a better in vivo model to study the tobacco risk continuum. Moreover, the commercially available system offers the benefits of being ready-to-use, robust, and reproducible with high throughput capacity that could be readily implemented by other labs to provide standardization across labs for collaborative and global studies in the future.
At Lifeline, we are always excited to share the latest research with the community on our blog. If you have used Lifeline cells and/or media in your research, we would love to hear from you.